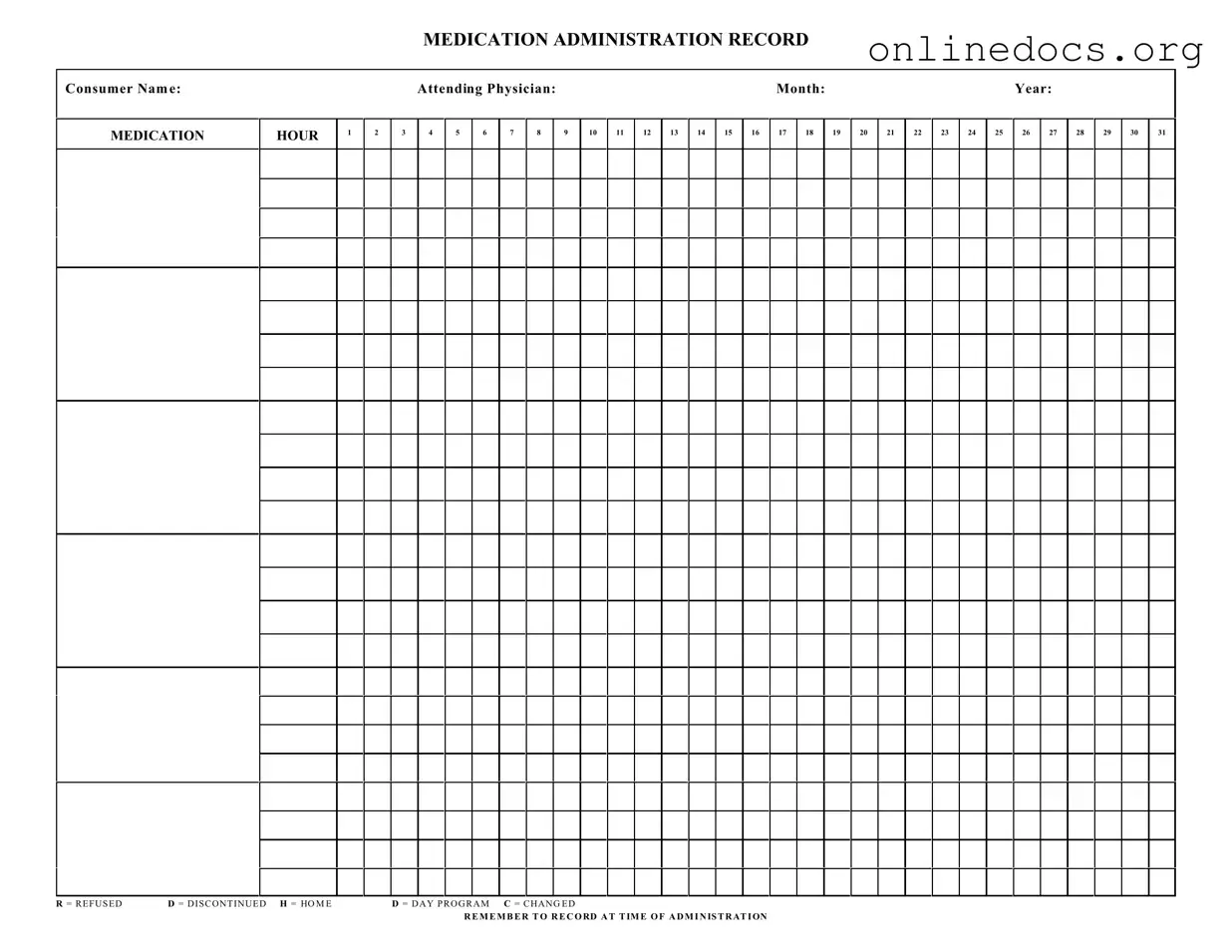
The Medication Administration Record (MAR) is similar to the Patient Medication Log, which serves as a comprehensive record of medications taken by a patient. Both documents track the administration of medications over time, ensuring that healthcare providers have a clear view of what has been prescribed and when it has been taken. The Patient Medication Log may also include additional details, such as side effects or patient-reported outcomes, which can enhance the understanding of a patient's response to treatment.
Another document that parallels the MAR is the Medication Reconciliation Form. This form is utilized during patient transitions, such as hospital admissions or discharges, to ensure that all medications are accurately documented and compared against the patient's previous medication list. Like the MAR, it aims to prevent medication errors and ensure continuity of care by confirming that patients receive the correct medications at all times.
The Treatment Administration Record (TAR) is also similar to the MAR. This document is often used in long-term care settings to record not only medications but also other treatments provided to patients. Both the TAR and MAR are essential for maintaining accurate records of patient care, and they help healthcare providers coordinate treatment plans effectively.
The Employee Handbook serves as a vital resource for employees, detailing essential information on company policies and workplace procedures. For a comprehensive understanding, employers may refer to additional resources such as the legalformspdf.com which provides valuable templates and guides related to employee handbooks.
The Nursing Care Plan shares similarities with the MAR as it outlines the specific medications and treatments a patient will receive based on their individual care needs. Both documents are integral to patient care, ensuring that nurses and other healthcare professionals follow the established protocols for medication administration and monitor patient responses accordingly.
The Prescription Record is another document that aligns with the MAR. This record details the medications prescribed to a patient, including dosage and frequency. While the MAR focuses on the administration of those medications, the Prescription Record serves as a foundational document that informs the MAR and helps track changes in medication therapy over time.
The Medication Administration Policy is also comparable to the MAR, as it outlines the procedures and guidelines for administering medications within a healthcare setting. While the MAR is a specific record for individual patient medication administration, the policy provides the framework that governs how those records are maintained and ensures compliance with regulatory standards.
Lastly, the Adverse Drug Reaction (ADR) Report is similar in that it documents any negative responses a patient may have to medications. While the MAR tracks the administration of medications, the ADR Report focuses on the outcomes of those medications. Both documents are vital for patient safety and contribute to the overall quality of care by identifying and addressing potential issues related to medication therapy.