The North Carolina Living Will form is similar to the Advance Directive. An Advance Directive is a legal document that outlines an individual's preferences for medical treatment in the event they become unable to communicate their wishes. Like the Living Will, it can specify the types of medical interventions a person does or does not want, providing guidance to healthcare providers and family members regarding end-of-life care decisions.
The Healthcare Power of Attorney is another document akin to the Living Will. This form allows an individual to appoint someone to make healthcare decisions on their behalf if they become incapacitated. While the Living Will focuses on specific medical treatments, the Healthcare Power of Attorney grants broader authority to the appointed agent to make decisions based on the individual's wishes and best interests.
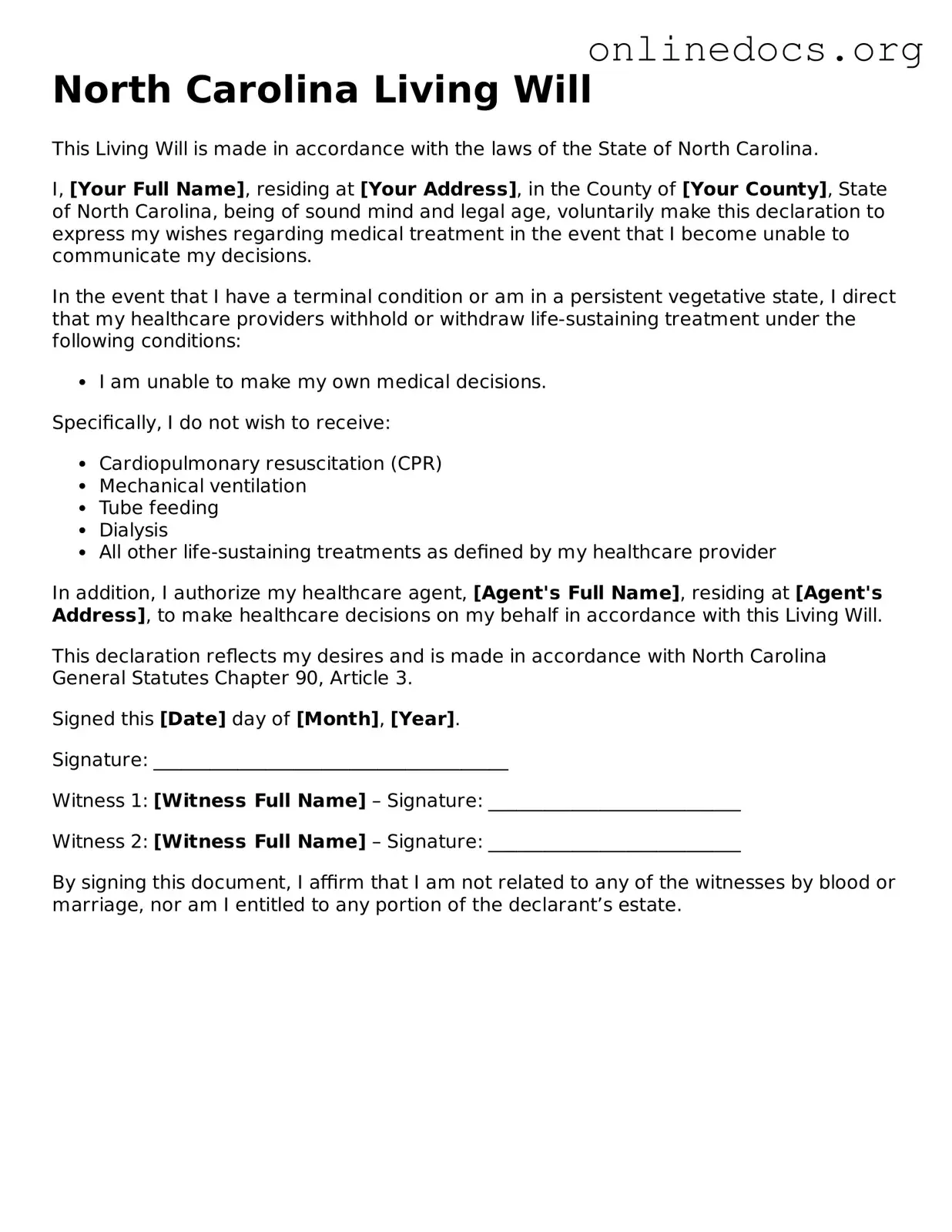
The Do Not Resuscitate (DNR) order shares similarities with the Living Will. A DNR order specifically instructs medical personnel not to perform cardiopulmonary resuscitation (CPR) if a person's heart stops beating. This document reflects a person's wishes regarding resuscitation efforts, aligning with the end-of-life decisions outlined in a Living Will.
For parents considering legal options regarding their children's welfare, it's important to explore various documents that can grant necessary authority during critical situations. One such option is the https://californiapdfforms.com/power-of-attorney-for-a-child-form/ which allows a designated adult to make decisions on behalf of a minor, ensuring that the child's needs are met during times of absence or incapacity of the parent.
The Physician Orders for Life-Sustaining Treatment (POLST) form is also comparable. POLST is a medical order that translates a patient's preferences regarding life-sustaining treatments into actionable medical orders. Like a Living Will, it addresses specific interventions, but it is typically used for individuals with serious health conditions, ensuring their wishes are honored in emergency situations.
The Durable Power of Attorney for Health Care is another document that parallels the Living Will. This form allows an individual to designate a person to make health care decisions on their behalf, similar to the Healthcare Power of Attorney. However, the Durable Power of Attorney can also encompass financial decisions, providing a broader scope of authority while still focusing on healthcare preferences.
The Mental Health Advance Directive is similar to the Living Will in that it allows individuals to express their preferences regarding mental health treatment. This document can specify treatment options, medication preferences, and appoint someone to make decisions in the event of a mental health crisis. It ensures that a person's wishes are respected during vulnerable times.
The Organ Donation Consent form shares a connection with the Living Will. This document allows individuals to express their wishes regarding organ donation after death. While the Living Will focuses on medical treatment preferences during life, the Organ Donation Consent form addresses decisions that affect what happens after death, aligning with a person's overall healthcare philosophy.
The Declaration for Mental Health Treatment is another document that resembles the Living Will. This declaration allows individuals to outline their treatment preferences in the event they are unable to make decisions due to mental illness. It provides guidance to healthcare providers and family members, similar to how a Living Will addresses end-of-life care preferences.
Lastly, the End-of-Life Care Plan can be seen as similar to the Living Will. This plan encompasses a broader range of considerations, including medical, emotional, and spiritual preferences for end-of-life care. While the Living Will focuses on specific medical interventions, the End-of-Life Care Plan may include additional aspects such as pain management, hospice care, and personal wishes, providing a comprehensive view of an individual's desires at the end of life.